Exemplars In Global Health. Why is under-five mortality important? https://www.exemplars.health/topics/under-five-mortality/what-is-under-five-mortality (2023).
Sharrow, D. et al. Global, regional, and national trends in under-5 mortality between 1990 and 2019 with scenario-based projections until 2030: A systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet Glob. Health 10, e195–e206 (2022).
Van Malderen, C. et al. Socioeconomic factors contributing to under-five mortality in sub-Saharan Africa: A decomposition analysis. BMC Public Health 19, 1–19 (2019).
Hall, S. et al. Government revenue and child and maternal mortality. Open Econ. Rev. 32, 213–229 (2021).
Hirschhorn, L., Sayinzoga, F., Beyer, C., Donahoe, K. & Binagwaho, A. (University of Global Health Equity, 2018).
Vikram, K. & Vanneman, R. Maternal education and the multidimensionality of child health outcomes in India. J. Biosoc. Sci. 52, 57–77. https://doi.org/10.1017/s0021932019000245 (2020).
United Nations Inter-agency Group for Child Mortality Estimation (UN IGME). Levels and trends in Child Mortality: Report 2021, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation. (United Nations Children’s Fund, New York, 2021).
Rahman, M. M., Ara, T., Mahmud, S. & Samad, N. Revisit the correlates of infant mortality in Bangladesh: Findings from two nationwide cross-sectional studies. BMJ Open 11, e045506 (2021).
Asif, M. F. et al. Socio-economic determinants of child mortality in Pakistan and the moderating role of household’s wealth index. BMC Pediatrics 22, 3. https://doi.org/10.1186/s12887-021-03076-2 (2022).
General Economics Division. Millennium Development Goals-Bangladesh Progress Report 2015. (Bangladesh Planning Commission, 2015).
Huda, T. M., Tahsina, T., Arifeen, S. E. & Dibley, M. J. The importance of intersectoral factors in promoting equity-oriented universal health coverage: A multilevel analysis of social determinants affecting neonatal infant and under-five mortality in Bangladesh. Glob. Health Action 9, 29741 (2016).
Patel, N. & Olickal, J. J. Maternal and child factors of under-five mortality in India. Findings from NFHS-4. Clin. Epidemiol. Glob. Health 12, 100866. https://doi.org/10.1016/j.cegh.2021.100866 (2021).
Binagwaho, A. et al. Exemplars in under-5 mortality: Bangladesh case study. (2019).
Rubayet, S. et al. Newborn survival in Bangladesh: A decade of change and future implications. Health Policy Plan 27(Suppl 3), iii40-56. https://doi.org/10.1093/heapol/czs044 (2012).
PMNCH, WHO, World Bank & AHPSR. Success Factors for Women’s and Children’s Health: Policy and Programme Highlights from Ten Fast-track Countries. (2014).
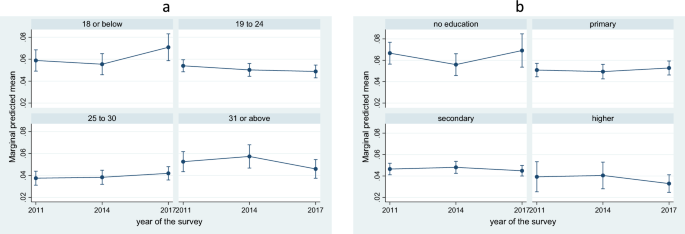
National Institute of Population Research Training – NIPORT, Ministry of Health Family Welfare & ICF. Bangladesh Demographic and Health Survey 2017–18. (NIPORT/ICF, Dhaka, Bangladesh, 2020).
National Institute of Population Research Training – NIPORT/Bangladesh, Mitra and Associates & ICF International. Bangladesh Demographic and Health Survey 2014. (NIPORT, Mitra and Associates, and ICF International, Dhaka, Bangladesh, 2016).
National Institute of Population Research and Training (NIPORT) & ICF. Bangladesh Demographic and Health Survey 2022: Key Indicators Report. (2023).
Akinyemi, J. O., Bamgboye, E. A. & Ayeni, O. Trends in neonatal mortality in Nigeria and effects of bio-demographic and maternal characteristics. BMC Pediatrics 15, 36. https://doi.org/10.1186/s12887-015-0349-0 (2015).
Khan, G. R., Baten, A. & Azad, M. A. K. Influence of contraceptive use and other socio-demographic factors on under-five child mortality in Bangladesh: Semi-parametric and parametric approaches. Contracept. Reprod. Med. 8, 22. https://doi.org/10.1186/s40834-023-00217-z (2023).
Khan, M. N., Trisha, N. I. & Rashid, M. M. Availability and readiness of healthcare facilities and their effects on under-five mortality in Bangladesh: Analysis of linked data. J. Glob. Health 12, 04081 (2022).
Rahman, A. E. et al. Child mortality in Bangladesh–why, when, where and how? A national survey-based analysis. J. Glob. Health https://doi.org/10.7189/jogh.11.04052 (2021).
The DHS Program. Mreging Datasets, https://dhsprogram.com/data/Merging-Datasets.cfm.
National Institute of Population Research Training – NIPORT/Bangladesh, Mitra and Associates/Bangladesh & ICF International. Bangladesh Demographic and Health Survey 2011. (NIPORT, Mitra and Associates, and ICF International, Dhaka, Bangladesh, 2013).
Alam, N., Van Ginneken, J. K. & Bosch, A. M. Infant mortality among twins and triplets in rural Bangladesh in 1975–2002. Trop. Med. Int. Health 12, 1506–1514 (2007).
Das, U., Chaplot, B. & Azamathulla, H. M. The role of place of delivery in preventing neonatal and infant mortality rate in India. Geographies 1, 47–62 (2021).
Kumar, S. et al. Handwashing in 51 countries: Analysis of proxy measures of handwashing behavior in multiple indicator cluster surveys and Demographic and Health Surveys, 2010–2013. Am. J. Trop. Med. Hyg. 97, 447–459. https://doi.org/10.4269/ajtmh.16-0445 (2017).
Huo, N. et al. Association of maternal body mass index with risk of infant mortality: A dose-response meta-analysis. Front. Pediatrics 9, 650413 (2021).
Sines, E., Syed, U., Wall, S. & Worley, H. Postnatal care: A critical opportunity to save mothers and newborns. Policy Perspecti. Newborn Health 1 (2007).
Sarkodie, A. O. Factors influencing under-five mortality in rural-urban Ghana: An applied survival analysis. Soc. Sci. Med. 284, 114185 (2021).
Abedin, S. & Arunachalam, D. Risk deciphering pathways from women’s autonomy to perinatal deaths in Bangladesh. Matern. Child Health J. 26, 2339–2345 (2022).
World Health Organization. Obesity: preventing and managing the global epidemic: Report of a WHO consultation. (2000).
The DHS Program. Guide to DHS Statistics, https://www.dhsprogram.com/publications/publication-dhsg1-dhs-questionnaires-and-manuals.cfm.
Rutstein, S. O. & Rojas, G. Guide to DHS statistics. Calverton MD ORC Macro 38, 78 (2006).
Kaombe, T. M. & Hamuza, G. A. Impact of ignoring sampling design in the prediction of binary health outcomes through logistic regression: Evidence from Malawi demographic and health survey under-five mortality data; 2000–2016. BMC Public Health 23, 1674. https://doi.org/10.1186/s12889-023-16544-4 (2023).
Carle, A. C. Fitting multilevel models in complex survey data with design weights: Recommendations. BMC Med. Res. Methodol. 9, 49. https://doi.org/10.1186/1471-2288-9-49 (2009).
Dotse-Gborgbortsi, W. et al. Spatial inequalities in skilled attendance at birth in Ghana: A multilevel analysis integrating health facility databases with household survey data. Trop. Med. Int. Health 25, 1044–1054 (2020).
Corsi, D. J., Neuman, M., Finlay, J. E. & Subramanian, S. Demographic and health surveys: A profile. Int. J. Epidemiol. 41, 1602–1613. https://doi.org/10.1093/ije/dys184 (2012).
Finlay, J. E., Özaltin, E. & Canning, D. The association of maternal age with infant mortality, child anthropometric failure, diarrhoea and anaemia for first births: Evidence from 55 low-and middle-income countries. BMJ open 1, e000226 (2011).
Fall, C. H. et al. Association between maternal age at childbirth and child and adult outcomes in the offspring: A prospective study in five low-income and middle-income countries (COHORTS collaboration). Lancet Glob. Health 3, e366–e377 (2015).
Katz, J. et al. Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: A pooled country analysis. Lancet 382, 417–425 (2013).
Kamal, S. M., Hassan, C. H., Alam, G. M. & Ying, Y. Child marriage in Bangladesh: Trends and determinants. J. Biosoc. Sci. 47, 120–139 (2015).
Islam, A. & Biswas, T. Health system in Bangladesh: Challenges and opportunities. Am. J. Health Res. 2, 366–374 (2014).
Balaj, M. et al. Parental education and inequalities in child mortality: A global systematic review and meta-analysis. Lancet 398, 608–620 (2021).
Mohamoud, Y. A., Kirby, R. S. & Ehrenthal, D. B. Poverty, urban-rural classification and term infant mortality: A population-based multilevel analysis. BMC Pregnancy Childbirth 19, 1–11 (2019).
Center on Society and Health. Why Education Matters to Health: Exploring the Causes, https://societyhealth.vcu.edu/work/the-projects/why-education-matters-to-health-exploring-the-causes.html#gsc.tab=0 (2015).
Health, T. L. P. Education: a neglected social determinant of health. Lancet Public Health 5, e361 (2020).
Rai, R. K., Singh, L. & Singh, P. K. Is maternal body mass index associated with neonatal mortality? A pooled analysis of nationally representative data from nine Asian countries. Nutrition 41, 68–72 (2017).
Johansson, S. et al. Maternal overweight and obesity in early pregnancy and risk of infant mortality: A population based cohort study in Sweden. Bmj 349, g6572 (2014).
Yang, Z. et al. Contribution of maternal overweight and obesity to the occurrence of adverse pregnancy outcomes. Aust. N. Z. J. Obstet. Gynaecol. 59, 367–374 (2019).
Melville, J. M. & Moss, T. J. The immune consequences of preterm birth. Front. Neurosci. 7, 79 (2013).
Balsells, M., García-Patterson, A., Gich, I. & Corcoy, R. Major congenital malformations in women with gestational diabetes mellitus: A systematic review and meta-analysis. Diabetes/Metab. Res. Rev. 28, 252–257 (2012).
Khashan, A. S. & Kenny, L. C. The effects of maternal body mass index on pregnancy outcome. Eur. J. Epidemiol. 24, 697–705 (2009).
Salihu, H. M. et al. Extreme maternal underweight and feto-infant morbidity outcomes: A population-based study. J. Matern.-Fetal Neonatal Med. 22, 428–434 (2009).
Perin, J. et al. Global, regional, and national causes of under-5 mortality in 2000–19: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet Child Adolesc. Health 6, 106–115 (2022).
Srivastava, S., Upadhyay, S. K., Chauhan, S. & Alagarajan, M. Preceding child survival status and its effect on infant and child mortality in India: An evidence from National Family Health Survey 2015–16. BMC Public Health 21, 1577 (2021).
Johns Hopkins Medicine. Complications of Multiple pregnancy, https://www.hopkinsmedicine.org/health/conditions-and-diseases/staying-healthy-during-pregnancy/complications-of-multiple-pregnancy (2023).
March of Dimes. Being pregnant with twins, triplets and other multiples, https://www.marchofdimes.org/find-support/topics/pregnancy/being-pregnant-twins-triplets-and-other-multiples (2023).
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. (World Health Organization, 2016).
Hakim, S., Chowdhury, M. A. B., Ahmed, Z. & Uddin, M. J. Are Bangladeshi healthcare facilities prepared to provide antenatal care services? Evidence from two nationally representative surveys. PLOS Glob. Public Health 2, e0000164 (2022).
Akter, E. et al. Levels and determinants of quality of antenatal care in Bangladesh: Evidence from the Bangladesh Demographic and Health Survey. medRxiv https://doi.org/10.1371/journal.pone.0269767 (2022).
Liu, L. et al. Global, regional, and national causes of under-5 mortality in 2000–15: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet 388, 3027–3035 (2016).
Bhutta, Z. A. et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost?. Lancet 384, 347–370. https://doi.org/10.1016/s0140-6736(14)60792-3 (2014).
National Institute of Population Research Training – NIPORT, Ministry of Health Family Welfare & ICF. Bangladesh Health Facility Survey 2017. (NIPORT – ICF, Dhaka, Bangladesh, 2020).
Kuhnt, J. & Vollmer, S. Antenatal care services and its implications for vital and health outcomes of children: Evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open 7, e017122 (2017).
Rai, R. K., Barik, A. & Chowdhury, A. Use of antenatal and delivery care services and their association with maternal and infant mortality in rural India. Sci. Rep. 12, 16490. https://doi.org/10.1038/s41598-022-20951-9 (2022).
Kim, E. T., Singh, K. & Weiss, W. Maternal postnatal care in Bangladesh: A closer look at specific content and coverage by different types of providers. J. Glob. Health Rep. 3, e2019004 (2019).
Hategeka, C., Tuyisenge, G., Bayingana, C. & Tuyisenge, L. Effects of scaling up various community-level interventions on child mortality in Burundi, Kenya, Rwanda, Uganda and Tanzania: A modeling study. Glob. Health Res. Policy 4, 16. https://doi.org/10.1186/s41256-019-0106-2 (2019).
Ministry of Health and Family Welfare. Operational Manual for Maternal and Newborn Health Service Accreditation Program. (2022).
RTM International. Assessment of Local Health Management Committees. (2012).